Policy
Strategic aim: Influence policy to ensure family needs are recognised and met.
We are fighting for better recognition at a policy level of the needs of families after ABI.
Download our evidence submitted to inform the ABI strategy.
Policy Connect: Joined Up Acquired Brain Injury Data for Better Care
On Tuesday, 13 May 2025, a Policy Connect meeting took place at Portcullis House, Westminster (Room T), chaired by Sir John Hayes MP, and held in partnership with the University of Essex. The focus was on how joined-up data can transform the understanding of Acquired Brain Injury (ABI) and uncover the hidden cost of ABI.
Chloe Hayward, Executive Director, United Kingdom Acquired Brain Injury Forum, kicked off the meeting with the wider context of the substantial and sustained efforts to achieve a nationwide ABI strategy and how the Policy Connect meeting could further advance this ambition. Discussions highlighted the critical gaps in data collection, post-discharge pathways, and public awareness. While much of the discussion was focused on gaps in data pertaining to those with ABI, discussions also emphasised the often overlooked, yet substantial, impact on families. Current healthcare models that focused too narrowly on the individual patient, rather than system-wide solutions that also addressed the needs of families and unpaid carers, were also criticised.
Read more about the event here: https://www.policyconnect.org.uk/events/joined-acquired-brain-injury-data-better-care
Engaging with Brain Injury: Summary of Two Policy Engagement Events.
by Aly Norman
Back in February, I wrote a short blog about an online event I hosted alongside a team of my fellow researchers and experts by experience from the NIHR funded Heads Together project. The event was designed to engage with policy makers across the South-West of England to discuss the societal and economic impact of acquired brain injury. This event was sponsored by the University of Plymouth policy engagement team and was a success with 44 interested people in attendance. The day consisted of outlining the journey that people with ABI go through after injury, through hospital services and into the community. The focus was on where the gaps in provision exist, where better support is needed, acknowledgement of the important role family members play in recovery, and the ongoing need to include them in conversations around care packages as well as considering their own wellbeing and mental health needs.
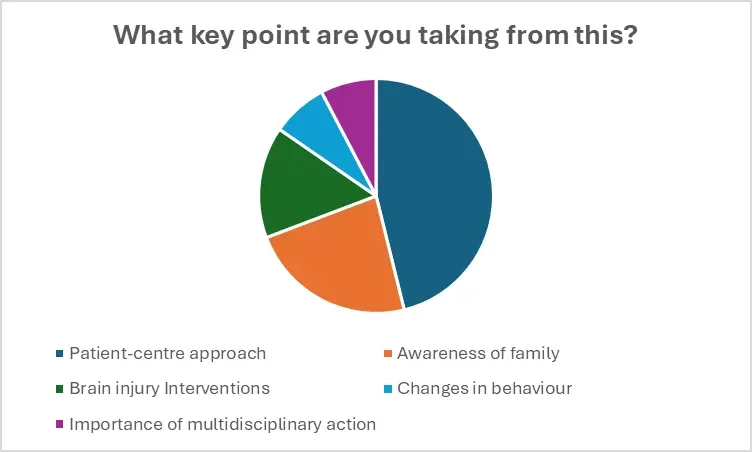
Throughout the initial day, attendees were given the opportunity to test their own knowledge of brain injury and to provide feedback on where they thought difficulties with service provision lay. As the figure below shows, attendees stated that the two key points of learning they had gained were around the need for a person-centred approach to care and the need for awareness of family members.
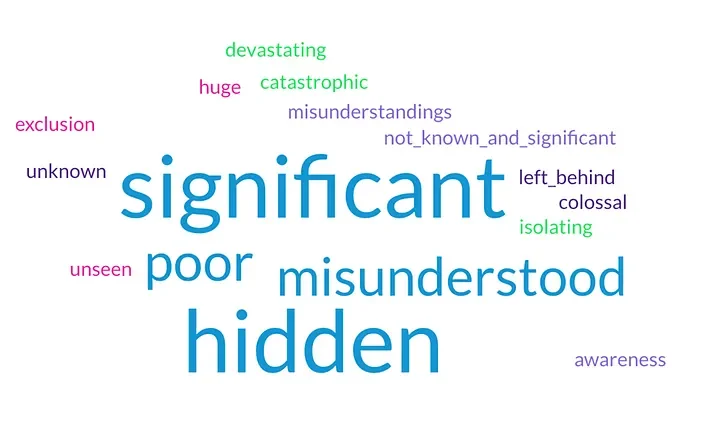
When asked to summarise the societal impact of brain injury in the UK, participants described it as ‘significant’ ‘hidden’ and ‘misunderstood’.
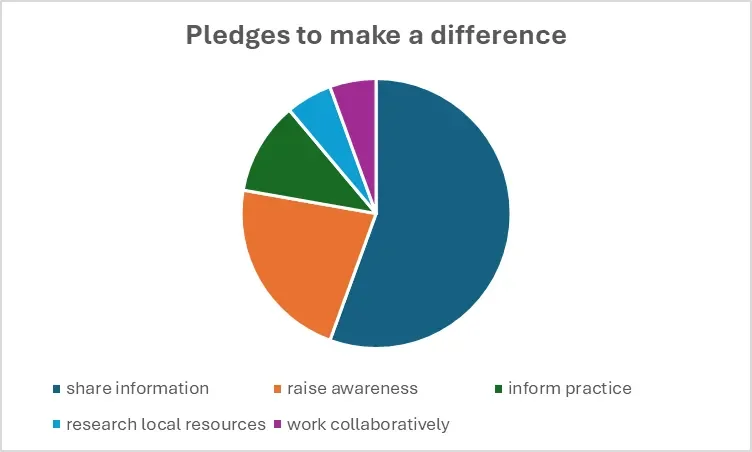
The event ended with attendees being asked to make a pledge about how they would attempt to do things differently in their workplaces to support people with ABI. Information sharing across organisations and about the needs of people with ABI and their families was the most common pledge stated (see right).
Since the online event in February, the team have been working hard to run a second in-person event sponsored by the University of Plymouth policy engagement team and the School of Psychology, and by Enable Law who provided catering and a wonderful venue for our event. On a lovely sunny day in Exeter, 36 individuals came together to talk about how to address the issues faced by people with ABI, and their families across the South-West of England, and beyond. The day was opened by Head First’s Dr Mark Holloway, a case manager, social worker and associate lecturer at the University of Plymouth. Mark discussed some of the headline figures associated with ABI, including the increased risks of mental health difficulties, substance misuses and suicide., He went on to outline the shocking statistics about the numbers of people with ABI within the criminal justice system (approximately 60%) and homeless communities (50%), all at a large cost to society and the UK taxpayer. I then went on to deliver some of the figures that are currently circulating about the economic impact of ABI, with figures for traumatic brain injury alone currently sitting at £22 billion. A new report by the United Kingdom Acquire Brain Injury Forum (UKABIF) is due to be released in Action for Brain Injury Week (Wednesday 21st May) that will outline that this figure is in fact much higher.
The next segment of the day was picked up by three of our fantastic experts by experience, Kate Mellor, Annie Ricketts and Emma Lucy Cole, telling their stories of being left without the care and support they need following their ABI.
Following the introductory talks, we moved on to the main segment of the day which was two workshops designed to focus on how to make improvements for people with ABI and their families. The first workshop, hosted by Dr Caroline Bald, University of Essex asked attendees to focus specifically on changes that they could make themselves or changes that their teams could make to improve life for people with acquired brain injuries. The attendees consisted of some policy makers, budget holders and professionals within the NHS, adult social care, housing and homelessness services and local South-West care providers.
We were lucky enough to have a brief presentation from Healthwatch Somerset who are currently compiling a report on the state of ABI care in Somerset, due to be release in Action for Brain Injury Week.
The day ended with a presentation from Chloe Hayward, CEO of UKABIF and the Brain Injury Social Work Group (BISWG) talking about the national picture and the work of UKABIF alongside the All-Party Parliamentary group for ABI who are currently working on a government strategy for ABI. Chloe presented on the economic cost report through UKABIF that was released on the 22nd May: https://cdn.ymaws.com/ukabif.org.uk/resource/resmgr/resources/the_cost_of_acquired_brain_i.pdf
Why the UK Must Put Informal Caring at the Heart of Policy: A Call to Action for 2025
by Aly Norman
In 2025, as the All-Party Parliamentary Group (APPG) for Acquired Brain Injury (ABI) intensifies its efforts to bring about meaningful change, there is one group that must not be overlooked: the UK’s unpaid, informal carers. Behind every person living with an acquired brain injury is often a partner, parent, sibling, or friend providing care. They are frequently unsupported, under-recognised, and increasingly at breaking point.
The Invisible Infrastructure of Care
Acquired brain injury affects hundreds of thousands across the UK, with far-reaching social and economic consequences. The APPG for ABI, formally inaugurated in March 2025, has committed to focusing on key priorities like access to rehabilitation, education, justice, and sports. Yet any conversation about brain injury must also recognise that the system often runs on the invisible labour of carers. These are usually family members who provide the critical support that the state simply cannot or will not.
These family members are the silent backbone of health and social care. They navigate complex systems, manage medications, provide emotional and physical support, and, often, do all this while sacrificing their own careers, health, and futures. One carer, supporting her husband after a stroke and previous brain injury, described dodging flu season while managing without respite or financial safety nets. Despite her full-time role, she doesn’t qualify for Carer’s Allowance because of restrictive eligibility rules — rules that haven’t meaningfully changed since the 1970s.
Carers Are Saving the State Billions
Research from Carers UK continues to show the harsh reality: carers are cutting back on essentials, facing poor mental health, and feeling abandoned by policymakers. According to the 2024 State of Caring survey:
68% of carers have reduced spending on leisure to cope financially.
Over 50% feel that their financial stress affects their mental health.
More than half report feeling overwhelmed “often” or “always.”
And yet, they continue. They care not just out of love, but because the alternatives are unthinkable. The cost of care services or residential placements far exceeds what the government spends on supporting these family members. And yet proposals now on the table threaten to cut an additional £500 million from financial support to carers by 2029. It’s a short-term saving that will cost us far more in the long run.
From Lived Experience to Political Action
Stories like that of Bill Revans, Local Liberal Democrat Councillor for Somerset Council who became a full-time carer after his wife’s ABI and cancer diagnosis, highlight how lived experience is beginning to shape political leadership. His journey from aspiring headteacher to elected official shows what’s possible when carers’ voices are amplified and respected. But for every carer who reaches public office, thousands more are struggling in silence.
That’s why it’s so significant that the Liberal Democrats have centred carers in their 2025 manifesto. Their proposals include raising Carer’s Allowance, introducing paid leave, guaranteeing respite, and giving carers legal protections. These are a blueprint that other parties must follow. These are not luxuries. They are the bare minimum if we are serious about a compassionate and functioning society.
A Turning Point for ABI and Care Policy
With the APPG on ABI re-energised and working on new evidence of ABI’s economic and personal cost, 2025 must be a turning point. Policymakers must not only listen to those with lived experience but act decisively. That means making informal caring central to UK policy. It means rethinking how we value care, who we support, and what kind of country we want to be.
It also means ensuring the voices of carers, who are often women and often older, often managing alone, are no longer ignored. If the Government is serious about “fixing social care” or “relieving NHS pressure,” it must start by properly recognising, supporting, and funding the work unpaid carers do every day.
What You Can Do
Everyone can play a part in demanding better.
Contact your MP and share your story or concerns.
Ask them to attend debates, push for reform, or visit local services.
Raise awareness online and in your community.
Support campaigns during ABI Awareness Week and beyond.
The APPG for ABI is providing a platform. But it’s up to all of us — carers, advocates, citizens — to make sure that 2025 becomes the year caring finally takes centre stage in UK policy.
Because no one should have to give everything and get nothing in return.