The cost of caring for families after ABI and the wrong kind of paradigm shift by Charlie Whiffin
I recently wrote a blog for the University of Derby in response to an article I read in The New England Journal of Medicine Catalyst reporting on a talk that called for a “paradigm shift” in how we define care in health systems and the idea of “empowering a hidden workforce.” The speaker argued that the definition of the healthcare workforce should include informal caregivers, family members, friends, and volunteers, in recognition of their vital yet often unacknowledged role in caregiving. While well-intentioned, I felt compelled to respond because the message risks systems offloading responsibility onto vulnerable, often traumatised family members, who take on their roles out of love and a sense of duty. This framing risks health and social care systems stepping further back instead of stepping up. The article overlooks some important points:
· Unpaid care is not the same as paid care — it comes with none of its rights nor protections.
· Task-shifting through upskilling informal carers is not the solution to a failing care system.
· Education on “how to care” is not enough — such education does not address the emotional, relational, and existential challenges that we know families face after ABI. My key takeaway in this blog is that families deserve, better than this. Families deserve real recognition and meaningful support, not to be rebranded as healthcare workers. A true paradigm shift would place families at the centre, not as an invisible resource, but as people with rights, needs, and voices of their own.
Read the blog in full here: https://www.derby.ac.uk/blog/posts/25/cost-caring-families-abi-wrong-paradigm-shift/
Progress and Challenges in ABI Rehabilitation: From Westminster to Local Action
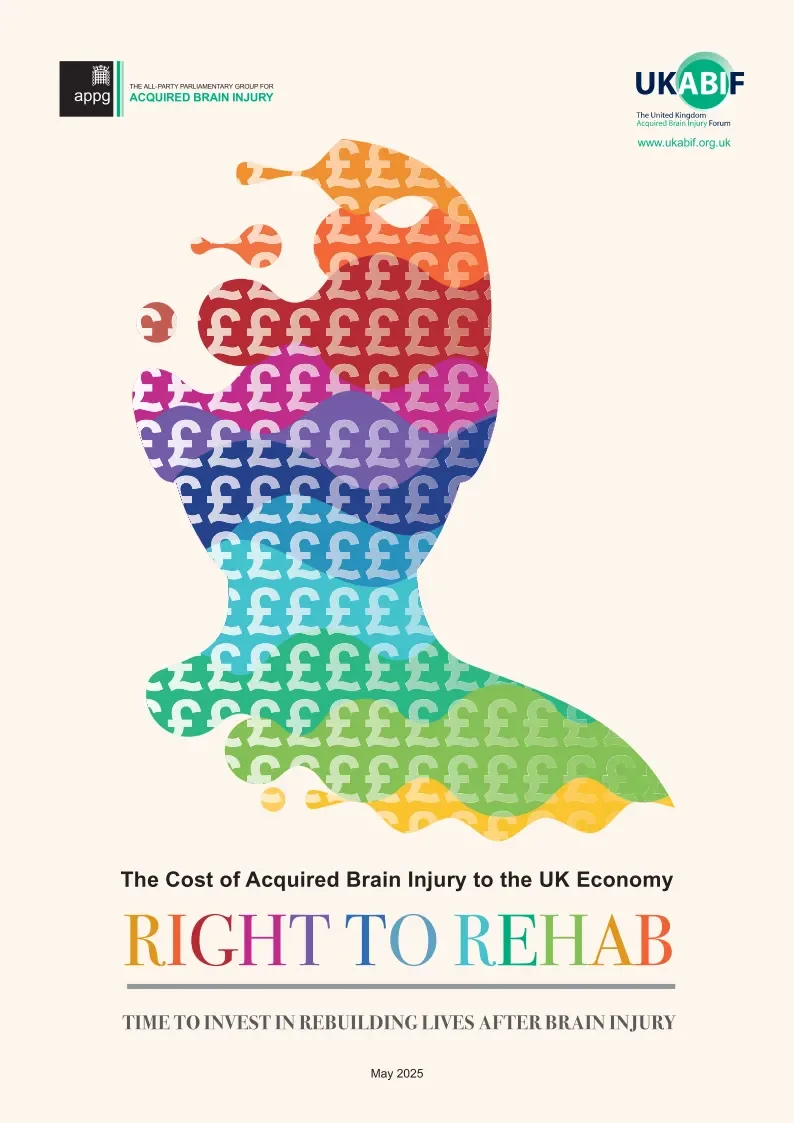
In July, key members of the United Kingdom Acquired Brain Injury Forum (UKABIF), alongside a range of stakeholders, attended the most recent meeting of the All-Party Parliamentary Group (APPG) for Acquired Brain Injury at Westminster. I was fortunate to be invited to present at this event, alongside Dr. Hope Kent from the University of Exeter, on the latest UKABIF publication — the Right to Rehab report.
Authored by Jennifer Misak, with contributions from many within the UKABIF team, the report highlights the significant economic cost of acquired brain injury (ABI) to the UK — estimated at £43 billion annually — and demonstrates how effective rehabilitation can reduce both the human and financial impact. I summarised some of these figures in a previous blog, so I will not repeat them here. Instead, I want to focus on the next steps: the APPG will reconvene in September with government ministers to develop a formal Action Plan addressing the issues raised in the report and drawing on its recommendations.
The report makes five key recommendations:
A statutory right to rehabilitation in every UK community
Establishment of sustainable funding mechanisms for community rehabilitation
Creation of a cross-Whitehall standing committee with a defined action plan
Improved data to support commissioning decisions
Systematic data collection across services
At the July event, Sir John Hayes also announced that Parliament will hold a further debate on brain injury and the urgent need for improved services. While the long-awaited ABI Strategy is still in development, this summer has felt like a small but important step forward in terms of national policy engagement.
That said, we must acknowledge the wider context. Even with greater political attention, we remain in an era of austerity where large-scale new investment in rehabilitation services is unlikely. This makes it vital for professionals in the field to consider alternative ways of improving outcomes for people with brain injuries and their families.
This was a central theme of the Southwest regional event held in Exeter in April, hosted by Enable Law and supported by the University of Plymouth. Local stakeholders, commissioners, and representatives from Headway groups came together to explore opportunities for collaboration and shared solutions. This kind of joint working will only become more important.
The NHS’ recently published 10-Year Plan proposes reducing the number of Integrated Care Boards (ICBs), meaning services will be commissioned at a broader regional level rather than county by county. For Headway groups, who operate as independent charities within individual counties, this shift highlights the need for greater cross-county collaboration to ensure services are effectively commissioned at the regional level. This change comes at a particularly challenging time, as many local Headway groups already face difficulties in maintaining local authority funding for social care provision.
Looking ahead, 2025 has brought positive momentum in national and regional conversations around ABI, but these developments must be viewed against a difficult financial backdrop. Progress will require new ways of thinking and smarter service delivery models. This may include embracing digital technologies to provide more cost-effective community-based rehabilitation, improving hospital-to-home transitions with greater involvement of families, and evidencing the value of services that reduce social isolation and support community reintegration after injury. The human and financial costs of loneliness and isolation are well-documented and cannot be ignored.
The road ahead is unlikely to be straightforward, and setbacks are inevitable. Yet, the need is clear, and the opportunity to make a difference is real. Personally, I am committed to continuing this journey — boots laced, ready to go the distance.
The Economic Impact of Brain Injury
Acquired brain Injury (ABI) is a collective term that refers to any injury that occurs to the brain caused during or after birth. The largest groups of these are traumatic brain injuries caused by external injury to the brain (through road traffic collisions, falls and assaults), strokes, and brain tumours. Figures for 2023–2024 show that there were 335,000 admissions to hospital with an acquired brain injury, and that there are an estimated two million individuals living with the long-term impact of ABI.
The symptoms of ABI include physical complications associated with mobility, speech and fatigue, emotional and behavioural difficulties such as anxiety, depression, and challenging behaviour, and cognitive difficulties such as memory impairments, difficulties with attention and concentration, with more subtle difficulties associated with executive impairments such as difficulties with planning, organising and initiating behaviour. This last group of symptoms can be particularly troubling for individuals with ABI and their families as they are completely hidden, can be difficult to spot without spending time with the person with ABI and can affect a person’s insight into their own disability. Yet, despite these figures and the impact on individuals and their families, those of us who have worked in the field for many years continue to be frustrated by the fact that ABI is viewed as a ‘niche’ topic that does not require much attention within either health or social care settings.
A new report, released today by Jennifer Misak, health economist at University College London, commissioned by the United Kingdom Acquired Brain Injury Forum (UKABIF), for which I am a trustee, outlines the economic impact of ABI in the UK. The report estimates that ABI costs the UK economy £42.6bn in 2023/24. Of this, £19.6bn was spent on health and social care services. A further £21.4bn was accrued through lost productivity.
Behind these headline figures sits the reality of life post-ABI. As well as the overall costs to health and social care, there is the impact on everyday life for both individuals and their families. The report suggests that a further £14.8bn comes from the costs of unpaid work lost among individuals, and a further £4.5bn from family carers. Separate wellbeing costs were estimated at £90bn, £43bn for individuals and 46bn for family carers. It is difficult to outline succinctly what this means for people living with the long-term consequences of ABI, but ultimately it leads to isolation, poor mental and physical health and relationship breakdown. These are all common issue that we see among family members who approach our organisation Anchor Point for guidance and information and is also reported by Headway groups across the country who support individuals with ABI.
This new report highlights that far from being niche, ABI is in fact a national problem with large societal and economic costs. It is also the leading cause of death and disability in people aged 0–40 years. I have worked as a researcher in ABI for nearly 20 years and during that time, my focus has been primarily on raising the profile of ABI among health and social care practitioners and with the public. As well as being a leading researcher in the field, I am also a family member.
My brother experienced a severe brain injury resulting from a road traffic collision. I was just 12 years old when my brother had his accident, thrown into a world of being a young carer. Despite working tirelessly to care for him and advocate for his needs, he eventually took his own life in 2014. A Safeguarding Adults Review, published by the Somerset Safeguarding Adults Board, concluded that mental health services within the local NHS trust, and adult social care failed to support his needs in a way that likely contributed to his suicide. Despite, training for professionals being one of the key recommendations from the review, there continue to be dearth of understanding in the Somerset area around ABI. I now work as a trustee for my local Headway group where we see clients coming through regularly who still struggle to have their needs met by services.
These struggles come with a cost. A cost that could be lower if services were better designed to support long term needs. This report highlights that this is a national picture across the UK. It is time that we stop viewing ABI through the lens of acute care, where we patch people up and send them home unsupported. We need an integrated care pathway that ensures people are passed through health and social care system more smoothly and with less wastage of time, effort and funds. The first step is to provide enhanced training for health and social care professionals to better understand and recognise ABI to ensure better access to services.
Why community matters for families post-ABI
Sue Jackson
Sadly, one of my husband’s longtime friends has passed away, so last week my husband and I went to his funeral. The church was packed and sitting at the back I could see how people were being affected by what had happened. They’d shown up to celebrate their friend’s life and to support his wife in the loss of her life partner.
In marriage, we learn how to live together. There are occasional upsets and tears over misunderstandings, but if we’re fortunate in our choice, we find someone with whom we’re a good fit and with whom we can relax and move through the space we share together with few pinches, no punches, and not too much in the way of bumping and barging either. Psychology tells us that most of what we do each day is done by rote or habit without us really having to think much about it. Something I call the ‘dance of the everyday’. Just as in a dance, we must learn the routine and how it fits with the pattern of the music and, if we have one, how our partner behaves (their strengths and weaknesses), so in life.
When One Person Is Injured, the Whole Family Feels It
When a loved one experiences a brain injury, the ripple effects are profound and often overwhelming. Recovery doesn’t just involve the person injured. It transforms the lives of everyone around them including spouses, children, siblings, and especially those who step into the role of carer. And yet, despite their central role in recovery, families are often left struggling in silence.
The State of Caring Survey is an annual research initiative conducted by Carers UK, aiming to capture the experiences and challenges faced by unpaid carers across the United Kingdom. As the most comprehensive study of its kind, the survey informs policy recommendations and advocates for better support for carers.
State of Caring Survey 2024:
The data below are some of the headline figures taken from the 2024 Caring Survey:
Financial Strain:
A significant portion of carers are struggling with daily living costs.
68% have reduced spending on hobbies and leisure activities.
60% have cut back on time spent with family and friends.
Over half (51%) report that their financial situation negatively impacts their mental health, with 61% feeling stressed or anxious about their finances.
Employment Challenges:
56% of working carers are hesitant to utilize their statutory right to Carer’s Leave due to concerns about the financial implications of unpaid time off.
Mental Health Concerns:
More than half (57%) of carers feel overwhelmed ‘often’ or ‘always’, indicating a rise in mental health challenges linked to the inability to take breaks from caregiving duties.
Future Aspirations:
In alignment with Carers UK’s 60th anniversary theme, “Equality: today and tomorrow,” carers expressed a desire for a future where they receive adequate support, recognition, and financial assistance.
These findings underscore the pressing need for comprehensive support systems that address the financial, emotional, and practical challenges faced by unpaid carers in the UK.
Brain Injury Changes Everything — Including the Caregiver
When someone experiences a brain injury, personality, memory, and behaviour can shift. Family members often become case managers, emotional anchors, advocates, and therapists — all while navigating their own grief for the life they once knew.
It’s no wonder caregivers face rising levels of stress, anxiety, and depression.
But what makes the difference?
Whether it’s peer support groups, employer flexibility, or government-backed financial aid, support systems are critical. A strong community can reduce isolation, share practical advice, and create space for caregivers to breathe.
More than anything, carers deserve to be seen, heard, and supported — not just during Brain Injury Awareness or Mental Health Awareness Week, but every single day. Because when we support families, we support healing. And when one person is injured, it’s the whole family that needs care.
Stronger Together: How Community Protects the Mental Health of Families After Brain Injury
Mental Health Awareness Week is an annual event in the UK, organised by the Mental Health Foundation, aimed at enhancing public understanding of mental health issues and promoting mental well-being. In 2025, the event is scheduled from 12 to 18 May, with the theme of ‘Community’.
The focus on ‘Community’ underscores the vital role that supportive networks play in maintaining and improving mental health. Being part of a safe and positive community provides individuals with a sense of belonging, safety, and purpose. Strong connections with others remind us that we are not alone, especially during challenging times.
When a brain injury strikes, it doesn’t just impact the individual — it ripples through the entire family. Roles within the family shift. Emotions run high. The future suddenly feels unfamiliar. Amid the whirlwind of medical appointments, rehab schedules, and hard conversations, one critical piece often gets overlooked, the mental health of the family. While there are many things that health professionals can do to mitigate the mental health impact on families, there is also an important role that community can play to offer protection.
Families of individuals with brain injuries often face a quiet storm, carrying an invisible weight of the impact of brain injury. People often experience grief for the person they knew. Stress is commonplace due to caregiving responsibilities. There is also anxiety about what comes next. That is a lot to expect any family to cope with. And when support is lacking at this crucial time, it’s easy to feel lost, isolated, and emotionally drained. But here’s the truth: No one should have to do this alone.
Community isn’t just something pleasant to enjoy. It isn’t just a bonus. It is a necessity, a lifeline. It protects mental health in ways that therapy, medication, and even the best resources sometimes can’t — because it brings human connection into the healing process.
Being around others who get it is healing. Being able to share stories with people who’ve walked a similar path brings comfort and removes the feeling that you’re “overreacting” or “not strong enough.” It says: “You’re not alone. What you’re feeling is valid.” Support groups often become unofficial guidebooks.Families swap tips on navigating medical systems, understanding legal rights, finding respite care, and surviving day-to-day life with a brain-injured loved one. It’s real-time, real-life knowledge you can’t find in a manual. Having people who just… listen — without trying to fix, judge, or minimize — is gold. Whether it’s a support group, an online forum, or a few close friends, that emotional safety net can be the difference between burnout and resilience. Finally, social connection fosters emotional resilience. When families feel seen, heard, and supported, they adapt better. They endure more. And they even begin to grow through their challenges.
Sometimes community shows up naturally, but most of the time it has to be built intentionally.
H
Here are a few places to start:
🧭 Join support groups — both local and online.
🧠 Connect with brain injury organisations — they often host events or peer mentorship programs.
🤝 Ask for help — from friends, neighbours, schools, churches. It’s okay to seek support.
💬 Start conversations — awareness grows when we talk.
A Word to the Rest of Us
If you’re a friend, coworker, neighbour, or simply someone watching a family go through this — know that you matter more than you think.
Drop off a meal.
Offer to babysit.
Send a “thinking of you” text.
Ask how they’re doing — not just how their loved one is.
Small acts of care create massive emotional relief.
Ultimately, brain injury recovery is a life-long marathon. This is true for the person with the injury and for the family. And no one should have to run that race alone. Community doesn’t make the hard parts disappear, but it can help to make them more bearable. It’s how we hold space for healing. It’s how we protect each other’s mental health. Because when we come together,
we don’t just heal — we heal stronger.
Throughout the week, various activities and resources will be available to encourage participation and raise awareness about the importance of community in mental health. Individuals and organizations are invited to share what community means to them using the hashtag #ThisIsMyCommunity on social media platforms such as Instagram, Facebook, X, and LinkedIn.
For more information on how to get involved and access resources for Mental Health Awareness Week 2025, visit the Mental Health Foundation’s official website.
On 15th November we held our Anchor Point Annual General Meeting. The Chairs, Professor Charlie Whiffin and Dr Alyson Norman, presented on the past year highlighting the achievements of our working groups. These have included a research publication currently being drafted for publication, YouTube research videos, information and education materials for families, best practice guidelines, letters-to-self project, engagement with policy and our new Anchor Point Strategy document.
The AGM was a chance to showcase the Letters-to-Self project which consists of a booklet of letters from family members to their past selves provided within a useful information resurce pack. We also revealed the Reflecting on Best Practice document that will form the basis of more consultancy work with healthcare professionals in the coming year. Our strategy document is now released and this will be circulated to all members via email. Finally, the AGM saw the soft launch of our new website. It still needs some updating and testing but will be made publicly available in due course. This will alow greater engagement with Anchor Point material.
The new year will bring a continued focus on reducing secondary trauma for families and a move towards charitable status with us registering as an unincorporated not-for-profit organisation.
Anchor Point Annual General Meeting

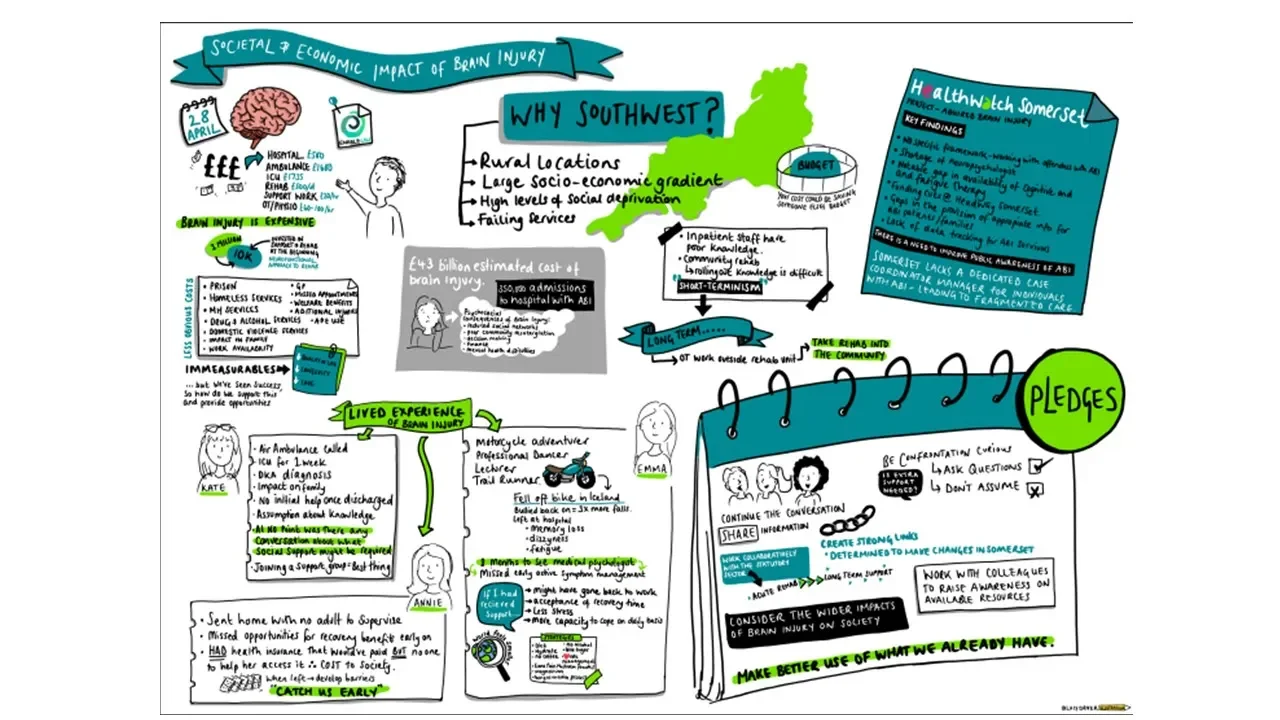
Societal and Economic Impact of Brain Injury
On Monday 10th February a team of researchers and experts by experience from the NIHR funded Heads Together project ran an online webinar for policy makers across the UK to come together and discuss the societal and economic impact of acquired brain injury. The day consisted of outlining the journey that people with ABI go through after injury, through hospital services and into the community.

Acquired Brain Injury Awareness Week
This week (15th — 21st May) is both Acquired Brain Injury (ABI) Awareness week and Mental health Awareness week. The theme of ABI week this year is every 90 seconds. This connects with the research conducted by Headway UK that demonstrates that every 90 seconds someone in the UK is admitted to hospital with a brain injury. The theme of mental health awareness week is anxiety.

UK Acquired Brain Injury Time for Change Summit 2024
Last week on the 4th November, the UK acquired Brain Injury Forum (UKABIF) hosted their annual Time for Change summit in Manchester. This long established event aims to raise awareness of the need to address issues around brain injury at a local and national level. This year many of the team from Anchor Point were present to listen to the talks and to present their own work.

Supporting Families After Brain Injury — Icanho, Shaftesbury
Shaftesbury Icanho specialises in acquired brain injury community rehabilitation for adults living across Suffolk who have sustained an acquired brain injury or stroke. We are a multi-disciplinary team that aims to provide a “whole family approach” for the rehabilitation of the person who has experienced the brain injury.

Supporting Families after Acquired Brain Injury at the Acute Care Phase
When a loved one sustains an acquired brain injury (ABI), it can be an overwhelming and traumatic experience for their family. The role of acute care staff extends beyond to providing crucial support and guidance to their families during this difficult time. Here are some ways healthcare professionals can help at this stage of the journey:

How can a UK Labour Government Address the Needs of Families After an Acquired Brain Injury?
In the UK, where the incidence of ABI remains high, it is crucial that the government in power has a robust and compassionate approach to healthcare and social support systems. On the lead up to the general election, Anchor Point showcased the manifestos of the major political parties to understand how they may support #FamilesAfterBrainInjury.

What can we learn from the RNLI and Mountain Rescue about how to put carers on the map?
For a long time after the stroke, he coped with the loss of his beloved mountains by avoiding them — he wouldn’t go anywhere that had mountains that he would once have been able to climb, and he avoided watching programmes about them on the television.

Respite care: to rest or not to rest? That is the question; and the only answer!
After decades of providing informal care, and over the last 3 years being an officially registered carer, l feel l’m at a critical stage of my life within my caring responsibilities. l have gained a useful and significant understanding of the ‘carer ecosystem’ and the myriad of support groups, activities, advice and guidance available to me in a local, regional and national level.

Reconnecting with the person before traumatic brain injury
When the brain is damaged, all these characteristics can be changed. This means that the person before the brain injury can be a completely different person after the brain injury. The physical changes can be more obvious, such as learning to walk or speak again.

Reflecting Family Experiences of Brain Injury in Party Manifestos: A Call to Action for the Next UK General Election
As the UK gears up for its next general election, it’s crucial to address the pressing issues faced by families dealing with the aftermath of brain injuries. Brain injuries not only impact individuals but also ripple through their families, affecting every aspect of their lives.

Carers need time for hobbies and a social life
It took a casual conversation with my friend’s Mum about what I’m up to these days, to make me realise that I’m no longer a wife, but a carer and that my once interesting life rich with travel, hobbies, and interests, has shrunk down to doing my job, housework and running around after my husband. I felt ashamed and close to tears having to admit that all that remains is my love of books because I can manage to fit a bit of reading in round everything else.

We Want to be Together: Supporting carers and those with Brain Injury through a United Front
Over the last several months Anchor Point has been posting about the need for the release of the ABI government strategy. As time goes on, we become ever more eager to understand the information that may be contained within this document. It is imperative that family members are included and recognized in terms of the contribution that they provide to supporting individuals with acquired brain injury.

What Families Want & Need Following Acquired brain Injury by Sue Jackson
I was summoned out of sleep by a ringing phone at 2am one morning to be told to get myself to the hospital where my husband was in A&E after a fall which had caused a serious brain injury. Fifteen years on, I still think about it — after all, while I wasn’t the one that fell and damaged my brain, the change to my husband was significant in ways that affected me and our life together.

ABI Strategy — looking forward to 2024
Previously I have written blogs about the eagerly anticipated ABI strategy. The latest news on this, which will come as no surprise to anyone given the date today, is that the strategy report will not be published this side of Christmas. Furthermore, due to cabinet reshuffles, there is yet another new minster in charge of the process. Progress has been slow and frustrating and certainly there is a feeling that the outcome may not be all we had hoped for.

The strategic vision for Anchor Point
Our second Annual general meeting took place on Thursday 12th October. There was a short report on the progress made over the last year by each of the seven individual working groups. The People group has now been chnaged to the Practice group to better reflect the group’s aims of understanding and promoting the best practice guidelines for the various health professionals who work with families after ABI.

The Acquired Brain Injury Strategy Post 2
As many people will already know, we here at Anchor Point are looking forward to the publication of the long-awaited ABI Government strategy. We still don’t know when this will take place, but it is anticipated before the end of the year. So why are we so keen on having an ABI government strategy and why is it so important for families?

Mental Health Awareness Day and #FamiliesAfterBrain Injury
In a recent Anchor Point meeting we had an important conversation about what the key message would need to be for professionals about life after brain injury for families. One of the really important points that came from that meeting linked to the idea of secondary impact.

The Acquired Brain Injury UK Strategy
There are very few people in the professional world of brain injury who aren’t aware of the current Acquired Brain Injury (ABI) strategy that is being worked on by Government. For those outside of the professional world, it is possible this is something that you have missed. The process of getting a strategy has been ongoing since 2021 and the report is due to be published ‘shortly’ according to Liz Truss, MP talking to NR Times in July.

Research in the area of Brain Injury: Why are families important
Within Anchor Point there are a series of different ‘working groups’ that focus on specific activities. One of these is the research group. This consists of a small number of individuals who are actively engaged in research within the area of brain injury, with a specific focus on family members. So what has the research field in this area got to say?

National Carers Week
This week (5th June — 9th June) is National Carer’s week. The theme for this year’s week is ‘visible, valued and supported.’ Through my work with Anchor Point and my work as a psychotherapist supporting family members whose loved one has had a brain injury, I know that the term ‘carer’ can seem quite contentious for them. The term carer doesn’t sit comfortably with family members a lot of the time, but after brain injury it can be even more complex.
Sign up to our mailing list
anchorpoint@ukabif.org.uk